DOI: 10.31038/PEP.2021242
Abstract
Background: Globally, health systems are optimistic about Coronavirus (COVID-19) vaccine introduction as one of the solutions for containment and elimination of the COVID-19 virus. However, the success of the vaccination efforts depends on the number of people who get vaccinated to reach herd immunity. Our study assessed the acceptability of the COVID-19 vaccine among Ugandans and the determinants for acceptability when the vaccine is made available.
Methods: Between October 6, 2020, and November 6, 2020, an anonymous web-based cross-sectional survey was conducted among Ugandans who could access an online semi-structured questionnaire designed using Google forms. The Google form was shared on email and social network platforms including Facebook, Twitter, Instagram, and WhatsApp. Participants that completed the survey received information encouraging them to spread the survey link to all their contacts.
Results: Overall acceptability of the COVID-19 vaccine was 396 of 604 (66%). Acceptability of COVID-19 vaccine was associated with having a Doctor of Philosophy (Ph.D.): APR: 2.90; 95% CI [1.33-6.45]. On the other hand, acceptability of COVID-19 vaccine was negatively associated with female sex: APR: 0.75; 95% CI [0.66-0.85], history of Adverse Events Following Immunization: APR: 0.63; 95% CI [0.42-0.96], not believing that COVID-19 is real: APR: 0.63; 95% CI [0.47-0.84] and not believing that COVID-19 has a vaccine; APR: 0.86; 95% CI [0.76-0.98].
Conclusions: Most participants indicated an intention to accept to receive the COVID-19 vaccine. However, addressing social demographic differences and health education is needed to increase the intention to receive the COVID-19 vaccine when available.
Keywords
Acceptability of COVID-19 Vaccine; COVID-19 vaccination; Health Belief Model; COVID-19 in Uganda
Introduction
The World Health Organization (WHO) declared the Corona Virus Disease 2019 (COVID-19) as a Public Health Emergency of International Concern (PHEIC) on 31th of January 2020, and finally a pandemic on 11th March 2020 [1]. As of September 23, 2020, there were 1,175,271 confirmed cases and 25,825 confirmed death due to COVID-19 in Africa [2]. The COVID-19 pandemic has had a huge impact across societies, with governments worldwide imposing restrictions of movement and other measures such as mandatory use of face coverings or quarantine to prevent the spread of the virus.
Most governments have pinned the hope of returning to normality on the availability of a COVID-19 vaccine [3]. As of November 6, Vaccine trials had reported encouraging results indicating that a COVID-19 vaccine is safe and produces a good immune response [4,5]. Despite being recognized as one of the most successful public health measures, vaccination is perceived as unsafe and unnecessary by a growing number of parents. Anti-vaccination movements have been implicated in lowered vaccine acceptance rates and the increase in vaccine-preventable disease outbreaks and epidemics [6]. The vast spread of COVID-19 misinformation could hinder the public acceptance of the COVID-19 vaccine [7].
Low-income countries like Uganda may not be able to afford to purchase vaccines for all its population. The COVAX plan is unlikely to be enough and Africa will have to be proactive in securing vaccines [8]. However, the success of a vaccination program will depend on the availability of vaccines for the vaccination program and the rates of uptake among the population. It is important to assess the public acceptance of the COVID-19 vaccine, factors for intention to accept or reject the vaccine, and willingness to pay for the vaccine among Ugandans to prepare and develop effective policies and messaging for vaccination now, to maximize uptake when a vaccine becomes available for Ugandans. In this study, we assessed, the acceptability of the COVID-19 vaccine among Ugandans, the determinants, barriers, and facilitators of acceptability of the COVID-19 vaccine.
Methods
Study Participants and Survey Design
Between October 6, 2020, and November 6, 2020, an anonymous web-based cross-sectional survey was conducted in Uganda. The researchers used a semi-structured questionnaire designed using Google forms. This helped generate a link that was shared on email and social network platforms like Facebook, Twitter, Instagram, and WhatsApp. Using online social media networks was appropriate during this period because of the COVID-19 lockdown and movement restrictions in Uganda. The survey targeted potential respondents of up to 1,000 and 641 were reached. Of these, 604 respondents completed all survey questions and provided written informed consent online. Only participants that were Ugandan residents who had internet access and aged above 18 years were included in the study. Participants that completed the survey received information encouraging them to spread the survey link to all their contacts. The questionnaire was pretested to a similar population and similar observations of the pretested population were eliminated from data analysis.
Instruments
A semi-structured and self-reported survey questionnaire was used to solicit data from participants. This contained informed consent, socio-demographic background, trust issues relating to COVID-19, information source, COVID-19 Beliefs, and COVID-19 vaccine acceptability.
Socio-demographic Measures
Information on sex, residence, marital status, religion, job category, education, and employment status were collected.
COVID-19 Beliefs
The Health Belief Model constructs were used to measure the Beliefs and attitudes [9,10]. Each construct of the model was measured using two questions assessed on a five-level Likert scale; Perceived Susceptibility (you have high chances of getting COVID-19 and the nature of your work puts you at a higher risk of getting COVID-19); Perceived Severity (you can get incapacitated if you contracted COVID-19 and you can die if you contracted COVID-19) Perceived Benefit (vaccination with safe COVID-19 vaccine will safeguard you from COVID-19 and Life will get normal if people get vaccinated) Perceived Barriers ( getting COVID-19 vaccine may put you in danger and vaccines are safe for human use); and Cues to Action ( discovery of COVID-19 vaccine makes you want to get it and trust of Information from MoH).
Acceptability of COVID-19 Vaccine
The outcome variable of this study was acceptability for the COVID-19 vaccine. It was measured using the question “Will you accept to receive the COVID-19 vaccine if it becomes available for use?” Acceptability of the COVID-19 vaccine was then computed as the proportion of people who self-reported having accepted the vaccine out of the total number of respondents.
Statistical Analysis
Data cleaning and analysis were performed using Microsoft Excel 2013 and STATA SE version 14 respectively. The results were described using measures of central tendency, dispersion, and associations. For continuous variables, like age, mean (and the standard deviation) was presented, for all categorical variables, frequencies, and percentages were presented. The outcome variable of this study was acceptability for the COVID-19 vaccine; which was computed as the proportion of people who self-reported to accept the vaccine if available out of the total number of respondents. Binary modified Poisson regression analysis was performed with a 95% confidence interval to determine significant associations between categorical dependent and independent variables.
Ethical Considerations
The study was conducted in adherence to the Institutional Research Ethics and the newly set guideline that adhere to UNCST COVID-19 Standard Operating Procedures. Personnel Identifiers of the respondents were not collected and there was no invasive procedure done on the participants. Formal ethical approval was granted by the Multidisciplinary Laboratory Technology Society Research, Science and Technology Committee, (Ref MLTS/RSTS/02/20). An online consent form documented the aims, nature, and procedure of the study. Anonymity and confidentially were strictly maintained. Respondents who didn’t consent to participate in the study were not able to access the rest of the questionnaire. While the respondents who consented to participate in the study were able to access the questionnaire and fill it out.
Results
The median (IQR) age of the study participants was 29 (25-33) years; with the majority aged 25-34 years. More so, more than half of the participants were male; 384 (63.6%), not married; 352 (58.3%), employed; 400 (66.2%) and resided in the central region; 348 (57.6%). About half of the participants had attained undergraduate education; 280 (46.4%) (Table 1).
Table 1: Socio-demographic characteristics.
| Characteristics | Frequencies (%)
n = 604 |
| Age
Median (IQR): 29 (25-33) years 20-24 years 25-29 years 30-34 years 35-39 years 40-45 years years |
138 (22.9) 200 (33.1) 145 (24.0) 58 (9.6) 26 (4.3) 37 (6.1) |
| Sex
Male Female |
384 (63.6) 220 (36.4) |
| Marital status
Married Not married |
252 (41.7) 352 (58.3) |
| Region of residence
Central Eastern Northern Western |
348 (57.6) 68 (11.3) 52 (8.6) 136 (22.5) |
| Education level
Secondary education Diploma education Undergraduate education Postgraduate education Ph.D. Education |
20 (3.3) 16 (2.6) 280 (46.4) 276 (45.7) 12 (2.0) |
| Religion
Anglican Catholic Pentecostal/born again Moslems Other religions |
220 (36.4) 184 (30.5) 132 (21.9) 40 (6.6) 28 (4.6) |
| Employment status
Employed Not employed Student |
400 (66.2) 48 (8.0) 156 (25.8) |
The majority of the participants had ever been vaccinated; 500(82.8%), had no history of Adverse Event Following Immunization (AEFI); 512 (84.8%); and more than half did not have a friend with a history of AEFI; 400 (66.2%). Majority of the participants perceived COVID-19 to be real; 520 (86.1%). About half believed that COVID-19 neither had a vaccine nor treatment; 288 (47.7%) and 288 (47.7%) respectively. More than half reported to observe COVID-19 ministry of health guidelines; 344 (57.3%) (Table 2).
Table 2: Knowledge and perceptions about COVID-19 vaccination.
| Characteristics | n (%) |
| Ever been vaccinated
Yes No Not sure |
500 (82.8) 76 (12.6) 28 (4.6) |
| History of AEFI
Yes No Not sure |
36 (6.0) 512 (84.8) 56 (9.2) |
| Known friend with AEFI
Yes No |
204 (33.8) 400 (66.2) |
| The perception that COVID-19 is real
COVID is real COVID is not real Not sure |
520 (86.1) 40 (6.6) 44 (7.3) |
| COVID-19 has treatment
Yes No Not sure |
124 (20.5) 288 (47.7) 192 (31.8) |
| COVID-19 has a vaccine
Yes No Not sure |
120 (19.9) 288 (47.7) 196 (32.5) |
| Observing Ministry of health guidelines
Yes No Sometimes |
344 (57.3) 8 (1.3) 252 (41.7) |
A higher percentage of participants trusted all the information sources except for social media and friends and families. A majority (83%) trusted information from international health organizations; followed by 79% who trusted information from the health care providers (Figure 1).
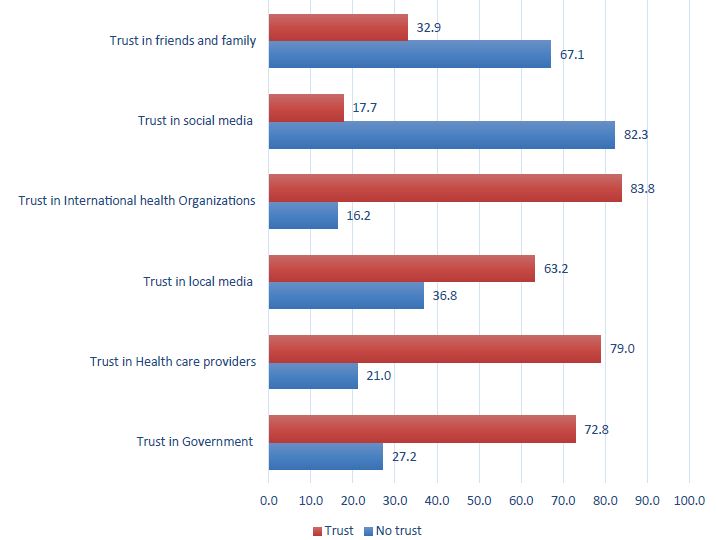
Figure 1: Percentage of participants with trust in COVID-19 information sources.
A higher percentage of participants perceived they were susceptible to COVID-19 [high chances of getting COVID-19 (75.5%) and work nature puts you at higher risk of getting COVID-19 (77.5%)]. A higher percentage also perceived that the COVID-19 vaccine will benefit them [vaccination will safeguard you from COVID-19 (72.3%) and life will get back to normal if people get vaccinated (73.6%)]. On the perceived threats construct, 39.5% of the participants perceived that the COVID-19 vaccine may be a threat to them while 80.4% perceived vaccines were safe for human use thus not a threat to them (Figure 2).
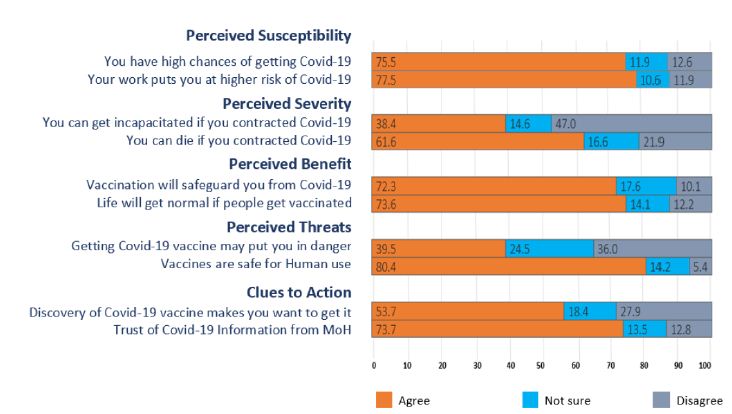
Figure 2: Percentage of Participants’ agreement with the Health Belief Model constructs.
Out of 604 complete responses, 396 (66%) of the participants indicated an intention to accept to receive the COVID-19 vaccine when it becomes available for use, and 208 (34%) indicated an intention not to accept (Figure 3).
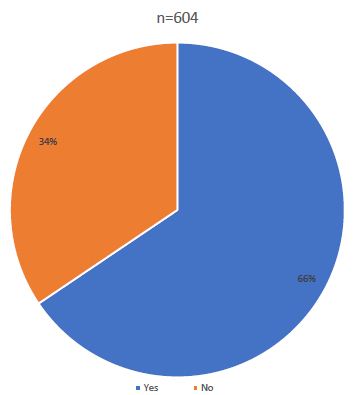
Figure 3: Percentage of Covid-19 Vaccine Acceptability among participants.
At multivariable analysis, the following factors were significantly associated with acceptability of COVID-19 vaccine: sex, education level, religion, history of AEFI, perception about COVID-19 and its vaccine, and trust in information from health care providers and the World Health Organization (WHO). There was a positive statistically significant association between acceptability of COVID-19 vaccine and Doctor of Philosophy (Ph.D.) education. Participants who had attained Ph.D. education were 2.9 times as likely to accept the COVID-19 vaccine compared to participants who had attained secondary education. (APR 2.90, 95% CI [1.33-6.45] ).
On the other hand, there was a negative statistically significant association between acceptability of COVID-19 vaccine and female sex, Catholic and Pentecostal religions, having a history of AEFI, the perception that COVID-19 is not real and has no vaccine, and lack of trust in health care providers and WHO.
Female participants were 25% less likely to accept the COVID-19 vaccine as compared to male participants, APR: 0.75; 95% CI [0.66-0.85]. Compared to Anglicans, Catholics and Pentecostals were 18% and 16% less likely to accept COVID-19 vaccine, APR: 0.82; 95% CI [0.73-0.92] and APR: 0.84; 95% CI [0.73-0.97] respectively. Participants who had a history of AEFI were 0.63 times as likely to accept the COVID-19 vaccine as individuals who did not have a history of AEFI, APR: 0.63; 95% CI [0.42-0.96]. Participants who didn’t believe that COVID-19 is real and those who didn’t believe that COVID-19 has a vaccine were 37% and 14% less likely to accept COVID-19 vaccine, APR: 0.63; 95% CI [0.47-0.84] and APR: 0.86; 95% CI [0.76-0.98] respectively. Finally, participants who didn’t trust information from health care providers and WHO were 0.75 times and 0.6 times as likely to accept the COVID-19 vaccine as participants who trusted information from health care providers and WHO, APR: 0.75; 95% CI [0.61-0.92] and APR: 0.60; 95% CI [0.45-0.79] respectively (Table 3).
Table 3: Bivariate Association for Variables Affecting the Intention to Accept COVID-19 Vaccine.
| Background characteristics | Acceptability of vaccine | Crude PR (95% CI) | Adjusted PR
(95% CI) |
||
|
Yes n=396 |
No n=208 |
||||
| Age
20-24 years 25-29 years 30-34 years 35-39 years 40-45 years years |
102 (25.8) 119 (30.1) 94 (23.7) 44 (11.1) 16 (4.0) 21 (5.3) |
36 (17.3) 81 (38.9) 51 (24.5) 14 (6.7) 10 (4.8) 16 (7.7) |
Ref. 0.81 [0.69-0.94]** 0.88 [0.75-1.02] 1.03 [0.86-1.22] 0.83 [0.60-1.15] 0.77 [0.57-1.03] |
|
|
| Sex
Male Female |
286 (72.2) 110 (27.8) |
98 (47.1) 110 (52.9) |
Ref 0.67 [0.58-0.78]*** |
Ref 0.75 [0.66-0.85]*** |
|
| Marital status
Married Not married |
172 (43.4) 224 (56.6) |
80 (38.5) 128 (61.5) |
Ref 0.93 [0.83-1.05] |
||
| Region of residence
Central Eastern Northern Western |
228 (57.6) 36 (9.1) 44 (11.1) 88 (22.2) |
122 (57.7) 32 (15.4) 8 (3.9) 48 (23.1) |
Ref. 0.81 [0.64-1.02] 1.29 [1.12-1.48]*** 0.99 [0.85-1.14] |
||
| Education level
Secondary Diploma Undergraduate Postgraduate PhD |
4 (1.0) 16 (4.0) 200 (50.5) 164 (41.4) 12 (3.0) |
16 (7.7) 0 (0) 80 (38.4) 112 (53.9) 0 (0) |
Ref 5.00 [2.08-12.02]*** 3.57 [1.48-8.61]** 2.97 [1.23-7.18]* 5.00 [2.08-12.02]*** |
Ref 2.06 [0.94-4.50] 1.82 [0.84-3.95] 1.43 [0.66-3.10] 2.90 [1.31-6.45]** |
|
| Religion
Anglican Catholic Pentecostal/born again Moslems Other religions |
168 (42.4) 112 (28.3) 68 (17.2) 28 (7.1) 20 (5.0) |
52 (25.0) 72 (34.6) 64 (30.8) 12 (5.8) 8 (3.8) |
Ref 0.80 [0.69-0.91]** 0.67 [0.56-0.81]*** 0.92 [0.74-1.14] 0.94 [0.73-1.20] |
Ref 0.82[0.73-0.92]** 0.84 [0.73-0.97]* 0.94 [0.71-1.24] 0.85 [0.70-1.03] |
|
| Employment status
Employed Not employed Student |
260 (65.6) 28 (7.1) 108 (27.3) |
140 (67.3) 20 (9.6) 48 (23.1) |
Ref 0.90 [0.70-1.15] 1.07 [0.94-1.21] |
||
| History of AEFI
No Yes Not sure |
348 (87.9) 12 (3.0) 36 (9.1) |
164 (78.9) 24 (11.5) 20 (9.6) |
Ref 0.49 [0.31-.0.78]** 0.95 [0.77-1.16] |
Ref 0.63 [0.42-0.96]* 0.97 [0.81-1.16] |
|
| COVID-19 is real
Real Not real Not sure |
372 (93.9) 20 (5.1) 4 (1.0) |
148 (71.2) 20 (9.6) 40 (19.2) |
Ref 0.70 [0.51-0.96]* 0.13 [0.05-0.32] |
Ref 0.63 [0.47-0.84]** 0.22 [0.09-0.55]** |
|
| COVID-19 has treatment
Has treatment No treatment Not sure |
68 (17.2) 196 (49.5) 132 (33.3) |
56 (26.9) 92 (44.2) 60 (28.9) |
Ref 1.24 [1.04-1.48]* 1.25 [1.04-1.51]* |
||
| COVID-19 has a vaccine
Has vaccine No vaccine Not sure |
84 (21.2) 188 (47.5) 124 (31.3) |
36 (17.3) 100 (48.1) 72 (34.6) |
Ref 0.93 [0.81-1.08] 0.90 [0.77-1.06] |
Ref 0.86 [0.76-0.98]* 0.92 [0.80-1.07] |
|
| Trust in social media
Has trust No trust |
82 (20.7) 314 (79.3) |
32 (15.4) 176 (84.6) |
Ref 0.89 [0.78-1.02] |
||
| Trust in HCP
Has trust No trust |
350 (88.4) 46(11.6) |
127 (61.1) 81 (38.9) |
Ref 0.49 [0.40-0.63]*** |
Ref 0.75 [0.61-0.92]** |
|
| Trust in WHO
Has trust No trust |
366 (92.4) 30 (7.6) |
140 (67.3) 68 (32.7) |
Ref 0.42 [0.31-0.57]*** |
Ref 0.60 [0.45-0.79]*** |
|
* <0.05; **<0.01; ***<0.001 level of significance AEFI-Adverse Events Following Immunization HCP-Health care providers, WHO-World Health Organization.
Discussion
The COVID-19 vaccine is considered one of the most outstanding ways to tackle the COVID-19 pandemic. However, the success of the vaccination efforts depends on the number of people who get vaccinated to reach herd immunity. Thus, it’s crucial to know and understand the acceptability of the vaccine and the factors that included an intention to accept the COVID-19 vaccine. Our study assessed the acceptability of the COVID-19 vaccine and the factors that influenced the intention to accept.
This study found the acceptability of the COVID-19 vaccine to be 65.6%. This is comparable to a survey conducted in 19 countries which found 71.5% of participants reported that they would be very or somewhat likely to take a COVID-19 vaccine [13]; a study in the USA where 69% of the adults indicated an intention to accept the COVID-19 vaccine; [11] a web-based study in Saudi Arabia that revealed 64.7% of participants indicated an intention to uptake the COVID-19 vaccine [12]; and a similar study in western Uganda that found 53.6% intention to accept covid-19 vaccine. Our findings are one of the first estimates of acceptability of a COVID-19 vaccine in Uganda and can be used together with other similar studies to guide projections of future vaccine uptake and as well understand the reasons for intentions to accept the COVID-19 vaccine.
Participants who had attained Ph.D. education were 2.9 times as likely to accept the COVID-19 vaccine compared to participants who had attained secondary education. This is comparable to a survey conducted in 19 countries which found higher levels of acceptability among participants with higher education [12]. This may be because they have a better understanding and exposure to relevant information regarding the COVID-19 vaccine. During the vaccine roll-out, government and health care providers and community-based social mobilization strategies will need to put more focus to provide more information to people with secondary education and below.
Female participants were 25% less likely to accept the COVID-19 vaccine as compared to male participants. This is similar to the study done in Congo which found more Male health workers were willing to accept COVID-19 Vaccine compared to females health workers [13]. Studies in the USA have indicated similar findings where men were more likely to accept the Covid-19 vaccine than women [11,14]. This could indicate that females may hesitate to receive the COVID-19 vaccine compared to males. Further studies on the general population and key populations may be needed to assess and understand COVID-19 vaccine acceptability [15].
Participants who had a history of AEFI were 0.63 times as likely to accept the COVID-19 vaccine compared to individuals who did not have a history of AEFI. This may be because of fear of suffering from another adverse reaction [16-18].
A higher percentage of participants perceived they were susceptible to COVID-19 and also a high percentage perceived that the COVID-19 vaccine will benefit them. This could explain the 65.6% acceptability of the COVID-19 vaccine [19-21].
Participants who didn’t believe that COVID-19 is real and those who didn’t believe that COVID-19 has a vaccine were 37% and 14% less likely to accept COVID-19 vaccine. This could be because of their lack of belief that COVID-19 is a serious public health threat to them thus the hesitancy to receive the COVID-19 vaccine.
Our study had some limitations in the design and data collection methods. We used a web-based questionnaire that required internet access and knowledge of how to read. This was because of the movement restrictions and government guidance on social distancing to reduce the spread of the COVID-19 virus. This may have led to selection bias against the individuals who couldn’t access the internet and couldn’t read the web-based questionnaire as reflected by the majority of the respondents having secondary education and above. However, the inference generated is important in the generation of a picture of the acceptability levels of the COVID-19 vaccine. Evidence from community survey which includes illiterate and non-illiterate class is key to assess sub-group acceptability levels without discriminating in access to web and internet devices.
We asked the participants to report their intention to receive the COVID-19 vaccine if the vaccine became available in the future. This was hypothetical; however, the true intention to take the COVID-19 vaccine may change when the vaccine is made available in Uganda.
We also registered a low response rate of 604 respondents making the findings less generalizable for the entire population in Uganda. Despite the limitations of our findings, our study is among the first studies to be conducted in Uganda and thus will provide a framework from which more studies will be conducted to better understand the acceptability for the COVID-19 vaccine among Ugandans and the determinants for acceptability of COVID-19 vaccine.
Conclusion
Most participants indicated an intention to accept to receive the COVID-19 vaccine. However, Policy Makers; governments; and Health Care Providers need to address Social demographic differences like sex, level of education, and religion, and their influence in intention to receive the COVID-19 vaccine. Other determinants for intention to receive the COVID-19 vaccine-like history of adverse reactions, knowledge on COVID-19 need to be addressed by right and targeted health education before mass vaccination campaign.
References
- Hua J, Shaw R (2020) Coronavirus (Covid-19) ‘infodemic’ and emerging issues through a data lens: The case of China. Int J Environ Res Public Health. [crossref]
- E. Programme,“COVID-19 COVID-19,” pp. 1-10.
- Sherman SM, et al. (2020) COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccines Immunother [crossref]
- Dagotto G, Yu J, Barouch DH (2020) Approaches and Challenges in SARS-CoV-2 Vaccine Development. Cell Host Microbe 28, no. 3, pp. 364-370. [crossref]
- Folegatti PM, et al. (2020) Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomized controlled trial. Lancet 396, no. 10249, pp. 467-478. [crossref]
- Dubé E, Vivion M, MacDonald NE (2014) Vaccine hesitancy, vaccine refusal, and the anti-vaccine movement: influence, impact, and implications. Expert Review of Vaccines. [crossref]
- Pennycook G, McPhetres J, Zhang Y, Lu JG, Rand DG (2020) Fighting COVID-19 Misinformation on Social Media: Experimental Evidence for a Scalable Accuracy-Nudge Intervention. Psychol Sci 31, no. 7, pp. 770-780. [crossref]
- Sisay OB, Smith E, Crone DD, Andersen H, Mamo LT, “A Covid-19 Vaccination Plan for Africa.”
- Coe AB, S. B. S. Gatewood, Moczygemba LR, J.-V. “Kelly” R. Goode (2012) The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Inov Pharm 3, no. 2.
- Costa MF (2020) Health belief model for coronavirus infection risk determinants. Rev Saude Publica 54, pp. 1-11. [crossref]
- Reiter PL, Pennell ML, Katz ML (2021) Acceptability of a COVID-19 vaccine among adults in the United States : How many people would get vaccinated ? Vaccine xxxx.
- Lazarus JV, et al. (2020) A global survey of potential acceptance of a COVID-19 vaccine. Nat Med [crossref]
- Nzaji MK, Ngombe LK, Mwamba GN, Miema JM, Lungoyo CL, Mwimba BL (2020) Acceptability of Vaccination Against COVID-19 Among Healthcare Workers in the Democratic Republic of the Congo. [crossref]
- Dustin Gibson, * Ph.D.; Smisha Agarwal1, 1, MBBS MBA Ph.D.; Ankita Meghani, Ph.D.;, P. M. M. Rupali J. Limaye, 1, 2 Ph.D., MPH, MA; Alain Labrique (2021) COVID-19 Vaccine Acceptability and Inequity in the United States: Results from a nationally representative survey.
- Power K, Power K (2020) The COVID-19 pandemic has increased the care burden of women and families and families. Sustain Sci Pract Policy 16, no. 1, pp. 67-73.
- Al-Wora Y, Ming L, Dhabali A, Al-Shami A (2021) Adverse reactions of COVID-19 vaccine among frontline workers in Fujairah, UAE. pp. 1-6.
- Mojamamy GM, Albasheer OB, Mahfouz MS (2018) Prevalence, knowledge, attitude, and practices associated with influenza vaccination among healthcare workers in primary care centers in Jazan, Saudi Arabia: A cross-sectional study. Trop J Pharm Res 17, no. 6, pp. 1201-1207.
- Khattak FA, et al. (2021) Prevalence of Parental refusal rate and its associated factors in routine immunization by using WHO Vaccine Hesitancy tool: A Cross-sectional study at district Bannu, KP, Pakistan. Int J Infect Dis 104, pp. 117-124. [crossref]
- Kim S, Kim S (2021) Searching for a general model of conspiracy theories and its implication for public health policy: Analysis of the impacts of political, psychological, structural factors on conspiracy beliefs about the covid-19 pandemic. Int J Environ Res Public Health 18, no. 1, pp. 1-28. [crossref]
- Attema A, L’Haridon O, Raude J, Seror V (2021) Beliefs and Risk Perceptions About COVID-19: Evidence From Two Successive French Representative Surveys During Lockdown. Front Psychol 12, no. February, pp. 1-16. [crossref]
- Karić T, Međedović J (2021) Covid-19 conspiracy beliefs and containment-related behavior: The role of political trust. Pers Individ Dif 175, no. January. [crossref]