Abstract
Background: Delayed Cord Clamping (DCC) has a known beneficial effect on the newborn, resulting primarily in an increase in iron levels of the newborn up to the age of six months. Despite the acknowledged advantages of delayed cord clamping, many surveys show that Early Cord Clamping (ECC) is in fact the technique most commonly used.
Goals: Identification of attitudes, knowledge and the behavior of midwives and gynecologists as regards cord clamping before and after a seminar on the subject.
Methods: The subjects were 62 midwives and 17 gynecologists who responded anonymously to a 24 item questionnaire examining their attitudes, knowledge and practice as regards cord clamping. The answers were on a scale of 1 to 4, where 4 represented “strongly agree” and 1 represented “do not agree”.
The questionnaires were distributed to the subjects at two points in time: a month before a programmed staff seminar on the subject, and a month after the aforementioned seminar. The results were analyzed by theoretical statistical methods, and relations were examined with Spearman’s coefficient.
Results: There was a significant difference (p = 0.03) between the perceived advisable time of delayed cord clamping before and after the seminar (3.14 minutes before and 4.52 minutes after). In clinical practice the average time of cord clamping was 2.7 minutes before the seminar and 4.1 minutes after (p = 0.02). A significantly statistical positive relationship (p = 0.000???) was found between the recommended time for cord clamping and the practice in the field.
Discussion: The seminar was effective in changing the attitudes of both midwives and doctors. This was especially true in clinical practice. A protocol for work in the delivery room was written on the basis of this research.
Scientific Background
Cord clamping is the most common intervention performed in the course of delivery. Until this occurs, placental blood flows from the placenta to the newborn in what is termed a “placental transfusion” [1]. This placental transfusion can increase the fetal blood volume [2]. In the course of the last decade, the question as to when to perform cord clamping has become a subject of great interest with disagreements on the optimal time to perform the clamping [1,3,4].
Already at the start of the nineteenth century a British physician by the name of Erasmus Darwin wrote:
“Another thing very injurious to the child is the tying and cutting of the navel string too soon which should always be left not only until the child has repeatedly breathed, but till all pulsations in the cord cease. As otherwise the child is much weaker than it ought to be, a portion of the blood being left in the placenta, which ought to have been in the child.”
At the start of the 1950s “Early” Cord Clamping (ECC) was defined as clamping within the first minute after birth. “Delayed” or “late” cord clamping was defined as clamping five minutes after delivery [5]. In 2013 the American Health Organization defined DCC as clamping performed one minute or more after delivery, or after the cessation of a pulse. Since 2014 the World Health Organization (WHO) has adopted this definition [6, 3] on the basis of the fact that this is the minimal amount of time necessary to improve maternal and fetal health [3].
This definition is based on the research of Ferrai et al, who found that 60% of the placental blood flows to the newborn in the first 60 seconds after birth. Most of the placental blood is transferred in the first 2 minutes after birth, and the flow of blood from the placenta to the newborn ceases within 3–5 minutes after the delivery. Thus the “placental transfusion” is completed in this time period. In the case of a term newborn, the placental transfusion adds from a quarter to one third of the child’s potential blood volume. The benefits, both immediate and long term, for the newborn have been reported in numerous studies [2]. The most obvious of these in term newborns is the increase in iron levels, which continues until the age of 6 months. The infusion of placental blood increase in the number of red blood cells [8], which in turn causes an increase in hemoglobin, hematocrit [9, 10] and ferritin [11]. This increase adds 50 mg/kg of iron to the baby, which is preserved for the first half year of life [12]. This prevents the development of anemia until it is possible to start feeding the child with iron rich foods [9, 10, 13].
The WHO’s recommendation on the optimal timing of cord clamping extends also0 to premature newborns. There are researchers who maintain that the benefits of DCC are especially true for premature babies [3] since DCC reduces the risk of intracranial bleeding by approximately 50% [14,15, 5]. Furthermore, the increase in blood volume is proportionately more since a premature baby’s blood volume is less to begin with, thus reducing even more the need to transfuse blood as treatment for anemia [14–16]. Furthermore, in the 25th to 31st week of pregnancy cord blood is rich in hematopoietic, or stem cells, and therefore ECC will lead to a low level of stem cells, thus increasing the chance of infection. As opposed to this, DCC will have a protective effect against infection in low birth rate newborns [17].
In research by Mercer et al which included prematures at 32 weeks of pregnancy, the relationship between DCC and the development of sepsis was examined. The results show that DCC reduces the risk of sepsis. They hypothesized that even a small amount of blood supplied in DCC provides enough stem cells to assist the immune system [17].
There are disadvantages to DCC such as the fact that the increase in hemoglobin caused by the intervention increases the risk of development of physiological jaundice in the newborn. This jaundice occurs when the general bilirubin levels in the blood of the newborn are higher than 5 mg per dl due to the breakdown of the red blood cells. In other words, the more red blood cells there are, the higher the risk of developing jaundice [3]. A review of the literature which examined 1,762 newborns supports this. Their results show that in babies with DCC there is a significant rise in the number requiring light therapy as a result of jaundice [11]. However, in another review that examined 1,912 newborns in 15 clinical studies, no difference was found in the incidence of light therapy between the groups with DCC or ECC. Furthermore, in the DCC group there was significantly lower incidence of anemia along with an increase of the hematocrit, ferritin and iron [9]. Anderson et al reached similar conclusions in 400 term infants divided into 2 groups: the first with ECC (less than 10 seconds) and the second with DCC (more than 180 seconds). The results showed no relationship between time of cord clamping and the development of jaundice in the children.
A further disadvantage attributed to DCC is polycythemia, defined in newborns as a hematocrit above 65% [18]. The increase in the blood volume which is a result of DCC is likely to cause an increase in the hematocrit and the viscosity of the blood. This viscosity is likely to cause a decrease in the oxygen transportation and thus lead to respiratory distress in the newborn [11]. This hypothesis found no support in the research. In a Cochrane review from 2013 which included 5 papers with 2,000 subjects, the effect of DCC on the mother was examined, in particular in regard to bleeding after delivery. The results showed no significant differences in the incidence of postpartum hemorrhage (more than 1,000 ml) or regular postpartum bleeding (less than 500 ml) between groups with DCC or with ECC. Furthermore, there were no significant differences between the two groups in the incidence of manual lysis of the placenta, the need for blood transfusion or the length of the 3rd stage of delivery [19].
In spite of the benefits of DCC for the newborn, it appears from the examination of research that in fact ECC is practiced more frequently [20].
For example, in a review that examined the attitudes of 148 obstetrical staff members on the optimal time for cord clamping, the majority actually practiced cord clamping 20–40 seconds after delivery, and a minority performed cord clamping more than 2 minutes after delivery [21]. In another study 101 observations of midwives, obstetricians and family physicians showed that the obstetricians performed the highest rate of ECCs (1).
A survey of 43 doctors showed that they did not perform DCCs on premature newborns and reported that they were either not aware of the evidence on the advantages of DCC or that they thought that DCC would interfere with the care that the neonatologists needed to supply [22].
Aims
The purpose of this study was to examine the knowledge and attitudes of midwives as far as regards DCC before and after a seminar to improve their knowledge on the subject.
Methods
The population of the study included 79 midwives and obstetricians working in the delivery rooms of a large medical center in Israel. 78.5% 62 were midwives, and the rest (21.5%, [23]) were obstetricians. The average age was 43.6 years (range 31–67 years). The average professional experience was 11.7 years (range 3 months-43 years). Only 17.7% (14) had taken a course in natural delivery.
Research Tools
Due to a lack of existing questionnaires on the subject, we built one on the basis of the existing literature. This comprised 24 questions addressing knowledge of cord clamping (for example, “Immediate cord clamping is likely to cause anemia”), attitudes (for example, “I do not practice DCC because I don’t believe it has many advantages”) and practice (for example, “I practice DCC only if the woman requests it”). The answers were on a scale of 1–4, 1 being “do not agree” and 4 being “agree.” A further part of the questionnaire examined the recommended time of cord clamping compared to the actual time practiced. In this part the subjects were asked to estimate the time of cord clamping of their low risk deliveries in the past week. They were also asked what they believed to be the best time for cord clamping in these infants. The questionnaire was given validity by midwife experts in the field and a researcher knowledgeable and experienced in the building of questionnaires.
The questionnaire was presented to the subjects at 2 points in time: one month before the seminar on the subject and one month after. The seminar consisted of lectures together with slide shows and presentation of articles on the subject.
Process
After receiving permission from the Medical Center’s Helsinki Committee, the questionnaires were provided to the subjects. Anonymity was promised, and the process was repeated one month after the seminar.
Statistical Analysis
The results from the questionnaire were recorded on SPSS. They were examined by theoretical analysis and statistics which included comparison of the groups with a
Results
In a comparison of the desired time for cord clamping, we found that before the seminar the subjects thought that 3.14 minutes was the optimal time and after the seminar 4.52 minutes. This is a significant difference (p = 0.03). In fact, the average time at which they performed cord clamping before the seminar was 2.7 minutes and after the seminar 4.1 minutes (p = 0.02).
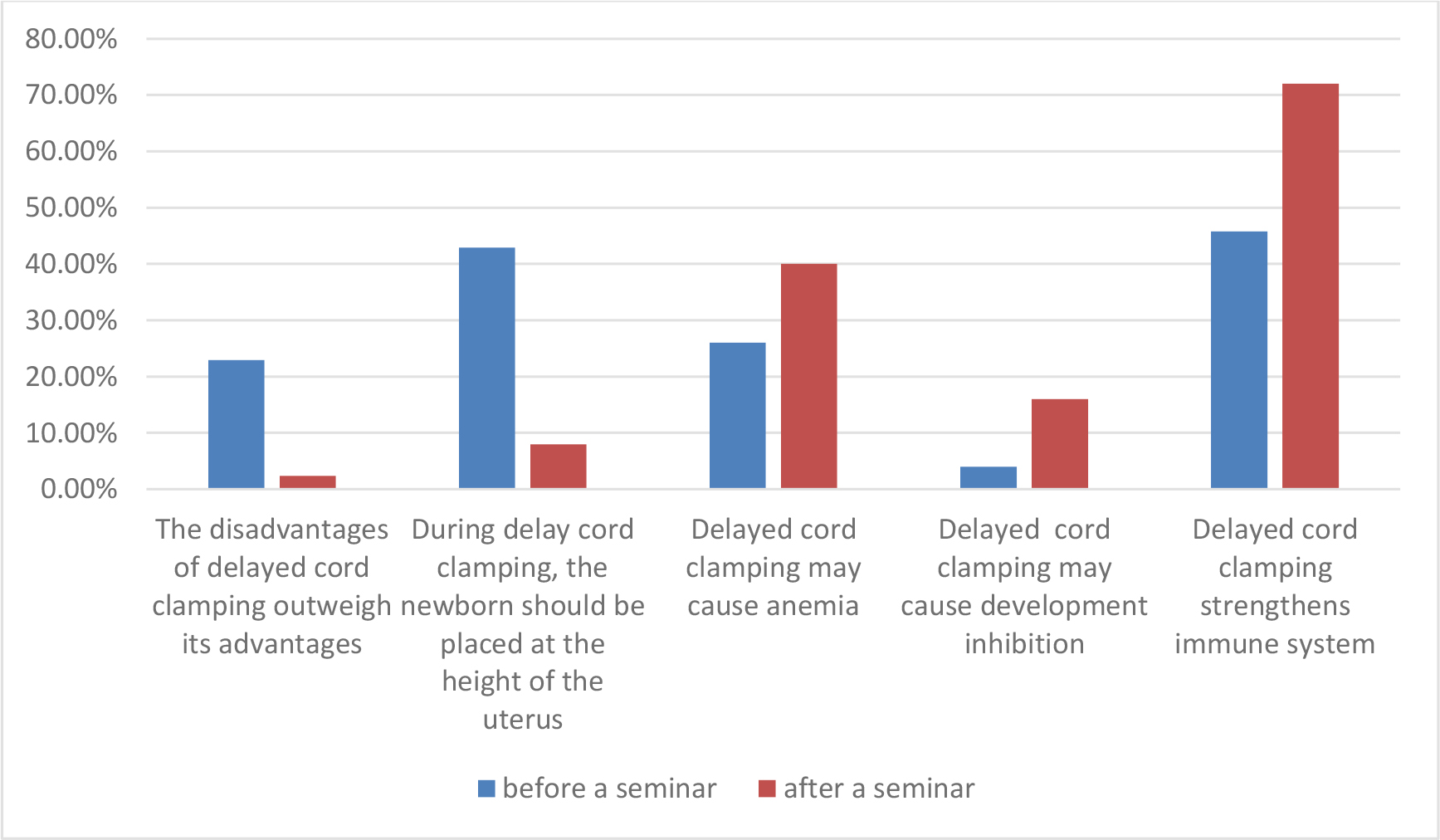
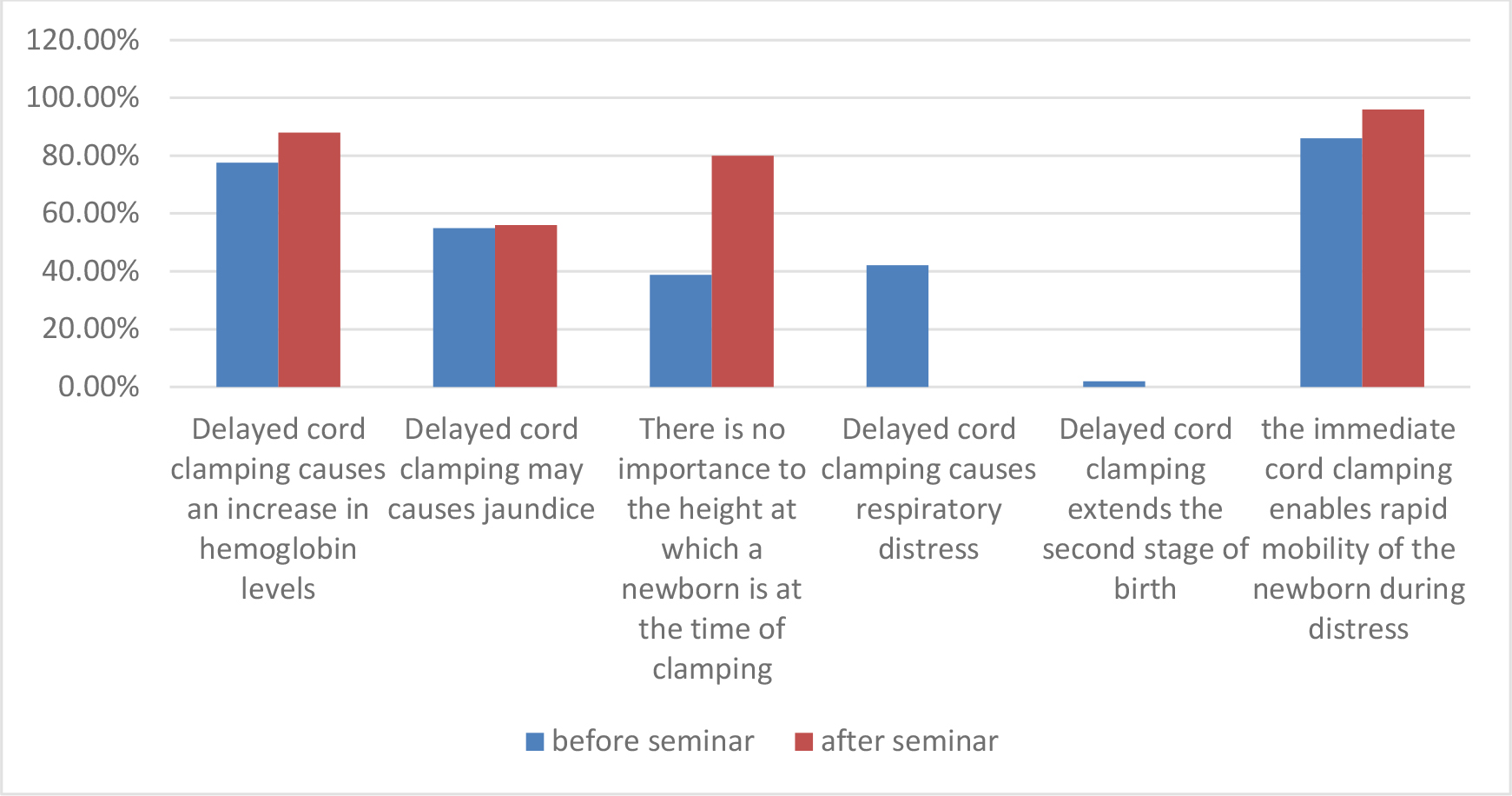
Before the seminar we found a positive significant relationship (P = 0.000) of average strength/power (r = 0.61) between the recommended time of cord clamping and the time of performance of cord clamping. It is interesting to note that after the seminar the relationship between the desired time of cord cutting and the actual time of cord cutting became even stronger (p = 0.000 and r = 0.85). Before the seminar about half of the participants reported that they did not have enough knowledge on the subject. As a result of the seminar there was significant increase in their knowledge of the subject: For example, before the seminar 42% answered incorrectly as to the position of a newborn in relation to the mother at the time of cord cutting. After the seminar 92% answered correctly (p = 0.003). Before the seminar only one half of the participants knew that DCC improves the immune system and after the seminar most of the participants were aware of this (p = 0.02, see graph1).
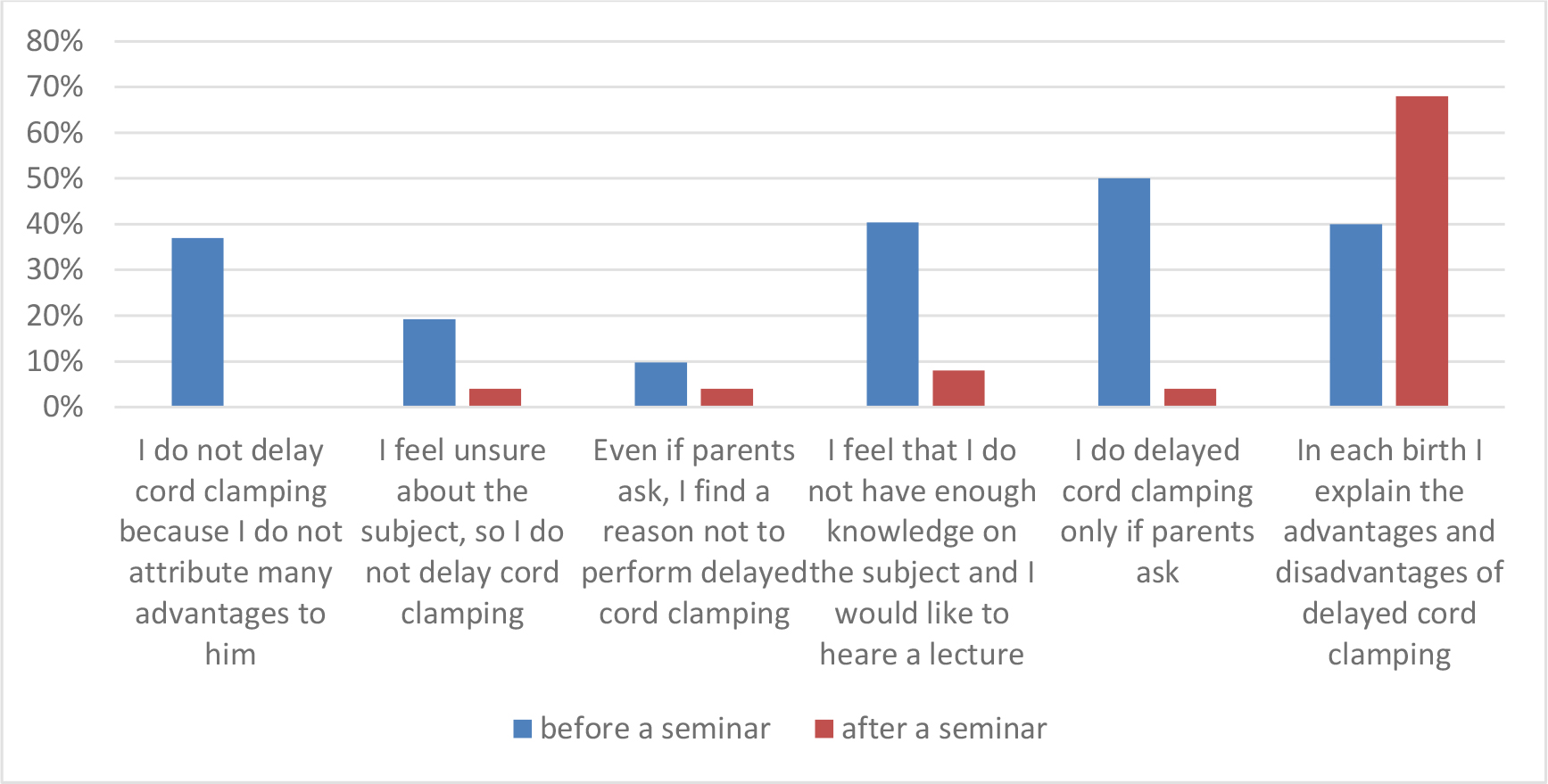
Graph 1
No differences were found in knowledge before and after the seminar as far as regards the length of the 3rd stage of labor and the development of neonatal jaundice. Levels of knowledge of this subject were high before and after the seminar. Before the seminar more than one third stated they did not perform DCC since they did not ascribe advantage to it, and after the seminar no participant answered thus (see graph 2).
Graph 2
Graph 3
In terms of knowledge, attitudes and time of cord clamping, no significant differences were found between the two groups of midwives and the physicians at the two points in time. The satisfaction of participants from the seminar on a scale of 1–10 was high (x = 9 S.D. = 1.09).
Discussion
The picture received from our research was that despite the large body of research presenting the advantages of DCC to the newborn [7], still many of the participants in our research did not ascribe importance of DCC before participation in the seminar. They also were not aware of the fact that DCC is responsible for increase in the iron of a newborn up to the age of 6 months [8, 12]. These results reinforce the results of many surveys that report on the fact that ECC is the most common practice [22]. However, there was no difference in the attitudes and knowledge as far as regards the possibility of the development of neonatal jaundice [3, 9, 11]. This finding is in accordance with the professional literature which presents conflicting results as to the timing of the cord clamping and the development of jaundice in the newborn [24, 25]. Participation in the seminar caused a significant change in understanding of the fact that DCC would cause respiratory distress of the newborn.
To summarize, the seminar was very effective in changing the attitude of midwives and obstetricians with regard to DCC. Furthermore, these new attitudes were then expressed in their clinical practice. One of the expressions of this was in the delivery rooms protocol for management of the 3rd stage of delivery, which was changed to reflect the new approach to DCC.
Recommendation
In light of the fact that research and our own experience shows that the common practice in deliveries is ECC, we recommend that ongoing education in a forum such as this seminar be considered for professionals in the field.
References
- Hutton E.K.,Stoll K., Taha N (2013) An Observational Study of Umbilical Cord Clamping Practices of Maternity Care Providers in A Tertiary Care Center. BIRTH 40: 39–451. [crossref]
- Farrar D, Airey R, Law G , et al (2011) Measuring placental transfusion for term birth : Weighing babies with cord intact. Br J Obstet. Gynecol 118:70–75
- World Health Organization (2014) Guideline: Delayed umbilical cord clamping: for improved maternal and infant health and nutrition outcomes.
- Jessica L. Bechard (2015) MSN RN : Delayed Umbilical Cord Clamping: Is It Necessary to Wait? International Journal Of Childbirth Education 30: 14 -16.
- Dunn PM. Dr Erasmus Darwin (1731–1802) of Litchfield and placental respiration. Arch Dis Child Fetal Neonatal Ed 88: 346–8.
- The American College of Obstetricians and Gynecologists (2012) Timing of Umbilical Cord Clamping After the Birth. Committee Opinion. 2012 Number 543.december 2012.
- Pan American Health Organization and World Health Organization Regional Office for the Americas. Beyond survival: integrated delivery care practices for long-term maternal and infant nutrition, health and development, 2nd ed. Washington, DC: Pan American Health Organization 2013.
- Strauss RG, Mock DM, Johnson K J, Cress GA, Burmeister L F, Zimmerman M, et al(2008) A randomized clinical trial comparing immediate versus delayed clamping of the umbilical cord in preterm infants: Short-term clinical and laboratory endpoints Transfusion, 658–665.48.
- Hutton E K, Hassan ES (2007) Late vs early clamping of the umbilical cord in full term neonates. Systematic review and meta- analysis of controlled trials. JAMA 297: 1241 -1252.
- Raju T, Singhal N (2012) Optimal timing for clamping the umbilical cord after birth. Clinics In Perinatology 39: 889 -900.
- McDonald SJ, Middleton P (2008) Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database of Systematic Reviews 2: CD004074.
- Eichen Eichenbaum-Pikser G, Zasloff, JS (2009) Delayed clamping of the umbilical cord: A review with implications for practice. Journal of Midwifery Women’s Health 54: 321–326.
- Van Rheenen P, Brabin BJ (2004) Late umbilical cord-clamping as an intervention for reducing iron deficiency anemia in term infants in developing and industrialized countries: a systematic review. Annals of Topical Paediatrics 24: 3–16
- Rabe H, Reynolds G, Diaz-Rossello J (2008) A systematic review and meta-analysis of a brief delay in clamping the umbilical cord of preterm infants. Neonatology 93: 138–44.
- Rabe H, Diaz-Rossello JL, Duley L, Dowswell T (2012) Effect of timing of umbilical cord 15. Clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database of Systematic Reviews 8: CD003248.
- Kugelman A., Borenstein-Levin L .,Kessel A., Riskin A., Toubi E., Bader D (2009) Immunologic and infectious consequences of immediate versus delayed umbilical cord clamping in premature infants :A prospective, randomized, controlled study. J. Perinat. Med 37: 281–287
- Mercer JS , Vohr BR, McGrath MM, Padbury JF, Wallach M ,Oh M. (2006) Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis :A randomized, controlled trial. Pediatrics 117: 1235–42.
- Sankar M, Agarwal R, Deorari A, Paul, V. (2010). Management of polycythemia in neonates. Retrieved from http://www.newbornwhocc.org pdf/Polycythemia_2010_200810.pdf
- McDonald SJ, Middleton P, Dowswell T, Morris PS (2013) Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes. Cochrane Database Syst Rev 7: CD004074.
- Winter C, Macfarlane A, Deneux-Tharaux C, Zhang W-H, Alexander S, Brocklehurst P et al. (2007) Variations in policies for management of the third stage of labor and the immediate management of postpartum hemorrhage in Europe. BJOG 114: 845–54.
- Sivaraman T & Arulkumaran S (2011) Delayed umbilical cord clamping : potential for change in obstetric practice. BJOG 118: 767.
- Ononeze ABO, Hutchon DJR (2009) Attitude of obstetricians towards delayed cord clamping: A questionnaire based study. J Obstet Gynecol 29: 223–224
- Haneline LS, Marshall KP,ClappDW (1996) The highest concentration of primitive hematopoietic progenitor cell in cord blood is found in extremely premature infants. Pediatric Res 39: 820–25.
- Jelin AC , Kupermann M, Erickson K, Clyman R, Schulkin J (2014) Obstetrician’s attitudes and beliefs regarding umbilical cord clamping. The Journal of Maternal-Fetal & Neonatal Medicine 27 : 1457–1461.
- Andersson O,Hellstrom- Westas L, Andersson D, Domellof M (2011) Effect of delayed versus early umbilical cord clamping on neonatal outcomes and iron status at 4 month : A randomized controlled trial. BMJ 343 : 7157