Introduction
Unintended pregnancy (both unplanned and unwanted) is a frequent public health problem worldwide [1,2]. It is estimated that in the Middle East and North Africa (MENA) region, one in four pregnancies is unintended. It is leading to unsafe abortions and jeopardizing the health and wellbeing of women and their families [3,4]. Dramatically, the World Health Organization (WHO) estimated that one woman dies every eight minutes due to unsafe abortion in developing countries [5]. Emergency contraception (EC) plays a vital role in preventing unintended pregnancy on 98% of occasions if applied correctly. Consequently, it helps to reduce unintended childbearing and unsafe abortion, which are major problems affecting maternal health [6]. The knowledge about back-up support and use of emergency contraception (EC) is the most important factor to prevent unplanned or mistimed pregnancies. EC is a type of contraception which is indicated after unprotected intercourse, following sexual abuse, misuse, or nonuse of contraception [7]. It includes the use of Emergency sexual Contraceptive Pills (ESCP), and/or the insertion of Intrauterine Device (IUD) [8]. Emergency contraception pills (ECPs) are also known as ‘the morning after pill’, ‘interception’, ‘post-coital contraception’ or ‘vacation pill’. ECPs include the use of a high dose of combined oral contraceptive pills (COCs) containing Ethinyl estradiol and levonorgestrel (the Yuzpe regimen) or the use of a high dose of Progestin-Only Pills (POPs) containing levonorgestrel. ECPs are effective only if used within 72 hours after unprotected sex. The effectiveness of ECP is 75% in the case of COCs and 85% in the case of POPs. ECPs can prevent pregnancy by delaying or inhibiting ovulation, prevent implantation, fertilization or transport of the sperm or ovum. ECPs do not interrupt or abort an established pregnancy. Once implantation has occurred, ECPs are not any more effective. Thus, ECPs do not cause any form of abortion or bring about menstrual bleeding [9–11]. Insertion of the intrauterine device (IUD) within seven days of unprotected intercourse has been reported as a highly successful method of post-coital emergency contraception. It prevents fertilization through the effect of Cu ions on sperm function and prevents endometrial receptivity [12,13]. Over the past years, contraceptives are available and well known in the Arab region [14]. However, emergency contraception is not widely known, and it not very commonly used. Most of the international studies focused on women’s attitudes towards and barriers to EC use [15,16].) Only a few studies have been conducted in developing countries, especially the Muslim world [17,18]. The first step towards understanding the use of EC is assessing local physicians’ knowledge of the methods and willingness to prescribe them. Based on this, we conducted this study to assess the knowledge, attitudes, and practice of primary health care centers physicians towards EC use.
Literature Review
In a study published from Egypt in 2012, by Shaaban et al., it was found that specialists’ knowledge was significantly high regarding the three most commonly used methods of EC: combined oral contraceptive method, progesterone-only pills (plan B) method and IUCD. The results of this study showed that only 39.5% of obstetrics and gynecology specialists and 24.0% of GPs/family physicians’ specialists and GPs/family physicians had a favorable attitude toward EC. 39.5% of specialists and 26.6% of GPs/family physicians reported ever prescribing EC. The combined oral contraceptive method was the most commonly prescribed method by specialists at 31.5%and GPs/family physicians at 27.0%. Age and years of experience significantly affected the three outcome measures [19].
In a teaching hospital in Karachi, Pakistan 2009, Abdulghani et al. reported that majority (71%) of the Family Physicians, including faculty physician, residents, and medical officers were familiar with emergency contraception, while 42% were not sure about the mechanism. Barriers to EC use were identified as religious/ethical reasons, liability, teratogenicity, and inexperience. Overall attitudes regarding emergency contraception were positive [20]. Another study conducted in 2005 by Sahin et al., in Maternal–Child Health/Family Planning Centers located in the European region of Istanbul, it showed that 82.9% of the family-planning providers including physicians, nurses and midwives were aware of emergency contraception correct description, time of administration and correct dosage of different method. 60% of them had accurately described the intrauterine device as emergency contraception. Most participants reported positive attitudes towards the need and use of Emergency contraception [21].
A study published in Saudi Arabia titled “One other side Emergency contraception: Awareness, attitudes, and barriers of Saudi Arabian Women” by Karim et al., conducted among 242 women showed that only 6.2% of the participants had some knowledge of EC and only two of them had ever used it. Health care professionals were the least reported source of EC information (6.6%, 1/15). The majority (73.3%) had a negative attitude toward EC being available over-the-counter without a prescription. The most common barriers to EC use were concerns about possible health effects. Only two women (13.3%) considered religious belief as a major hindrance to EC use. This study revealed that Health care professionals were the least reported source of information, which is a cause for concern. The major barriers identified for this were concerns of women about the possible side effects of EC and its health consequences. The authors in this study recommended that health care professionals should be encouraged to provide appropriate counseling services related to reproductive health in their consultations tailored to the country-level characteristics, in light of the social norms and religious values [22]. Another study from Saudi Arabia aimed to determine the knowledge, attitude, and practice of EC among Saudi women of childbearing age. This study included 370 women, with a mean age of 32.3 ± 6.3 years. Of these, 31.6% knew how to prevent pregnancy after unprotected sex, and 62 knew about EC, 67.7% thought EC should be widely advertised, and 48.4% thought it should be made available even without a prescription. Almost 76% said that they were not shy to ask for EC, and 59.7% claimed that both partners should decide about the use of EC. The most common reason for not using EC was medical concerns. The authors in this study concluded that among Saudi women, knowledge, awareness, and EC use remain low, although a positive attitude for future EC use exists [23].
In Iran, there is a study that reported EC knowledge and attitude scores of 69.4 ± 11.8 and 70.1 ± 12.8, respectively among health care providers. The providers’ knowledge score was good only in 35%, but the vast majority (95.7%) had positive attitudes [24].
Aims and Objectives
In this study, we aimed to assess the Knowledge, attitude, and practice of health care centers physicians about the commonly used types of emergency contraception (EC) methods.
Methods
This was a descriptive cross-sectional study that has been conducted in 11 Primary Health Care Centers in Prince Sultan Military Medical City, which is in Riyadh at the center of Saudi Arabia. The study population included Primary Health Care Physicians who worked at Prince Sultan Military Medical City, Irrespective of nationality, gender, age or type of education.
The sample size was calculated by using the equation:
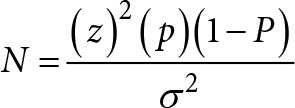
With considering a confidence level of 95 and a confidence interval of 5, the total population approximately 182. The sample size was 110, and by adding 10% of non-response or missing data, it ended with a sample size of 121. Data were collected by two methods: self-administered questionnaire and online Google form. The study was conducted during the period from February to March 2019 by using the random sampling technique. The questionnaire was developed by the researcher and supervisor after reviewing the previous similar researches. The questionnaire consists of five parts; the first part includes questions regarding personal data and occupation history (age, gender, marital status, nationality, job position, and the number of years in practice). The second, third, and fourth parts include questions about emergency contraception knowledge, practice, and attitude; respectively. The fifth part includes perceived barriers.
The questionnaire was reviewed for validation by three expert consultants in Family Medicine. A pilot study was done among 20 primary healthcare physicians to assess the understanding of questions and feasibility of the questionnaire. The knowledge questions were scored 1 for a correct answer and 0 for an incorrect answer for each question, and the total knowledge was converted to a percentage score where it was considered satisfactory if > or =70% and unsatisfactory if <70%. For attitude questions; they were scored on a scale from 1 to 5; where strongly disagree was scored 5 and strongly agree was scored 1. The total score was converted to a percentage score where it was considered positive if > or =70% and negative if <70%.
Statistical Analysis
SPSS statistical package for the social sciences software, version 25 was used for the statistical analysis. All categorical variables were expressed as frequencies and percentage and continuous variables were expressed as mean and standard deviation (SD). Appropriate statistics were used for categorical and continuous data, by chi-square and student t-Test. To study the relation between knowledge, attitude, and practice, and also to analyze the relationship between knowledge, attitude and practice of EC with demographic characteristics and occupational history of physicians (e.g.; age, gender, nationality, number of years in practice and area covered by physicians). A p-value of < 0.05 was considered statistically significant.
Results
(Table 1) Slightly more than half (51.2%) of the sample were males, and around half (43.8%) were in the age group of 20–29. Around three quarters (76%) of the sample were Saudi, and (14%) were Egyptians. The majority (66.1%) were married and around a quarter (26%) of the sample were junior residents, while 21.5% were senior registrar, and 19.8% were senior residents. The highest percent (77.7%) had national highest qualification while 13.2% had international, but not Western qualification and only 9.1% had Western qualification. More than half of the sample (54.5%) had 0–5 years of experience, while around the third (28.1%) had 6–10 years. Around half of the sample (43%) had 6–7 sessions per week, while 39.7% had 8–10 sessions, and only 17.4% had 0–5 sessions. More than 94% of the sample mostly cover the General Clinic GB, while 58.7% mostly cover the General Clinic GW. Data is shown in table one.
Table 1. Demographic characteristics and occupational history of the studied physicians (n = 121).
|
Items |
No. |
% |
|
Age(years): |
||
|
20–29. |
53 |
43.8 |
|
30–39. |
44 |
36.4 |
|
40–49. |
13 |
10.7 |
|
>=50. |
11 |
9.1 |
|
Gender: |
||
|
Male. |
62 |
51.2 |
|
Female. |
59 |
48.8 |
|
Nationality: |
||
|
Saudi. |
92 |
76.0 |
|
Egyptian. |
17 |
14.0 |
|
Sudanese. |
8 |
6.6 |
|
Bengalis, Pakistan, Jordanian, Syrian. |
4 |
3.4 |
|
Marital status: |
||
|
Single. |
39 |
32.2 |
|
Married. |
80 |
66.1 |
|
Widow. |
2 |
1.7 |
|
Position in the medical profession: |
||
|
Consultant. |
11 |
9.1 |
|
Senior registrar. |
26 |
21.5 |
|
Registrar. |
22 |
18.2 |
|
Senior house officer. |
6 |
5.0 |
|
Senior resident. |
24 |
19.8 |
|
Junior resident. |
32 |
26.4 |
|
Highest qualification achieved in: |
||
|
National. |
94 |
77.7 |
|
International, but not Western. |
16 |
13.2 |
|
Western. |
11 |
9.1 |
|
Years of experience: |
||
|
0–5. |
66 |
54.5 |
|
6–10. |
34 |
28.1 |
|
11–20. |
12 |
9.9 |
|
>20. |
9 |
7.4 |
|
The number of sessions per week: |
||
|
0–5. |
21 |
17.4 |
|
6–7. |
52 |
43.0 |
|
8–10. |
48 |
39.7 |
|
The area covers most of the times: |
||
|
General booked Clinic (GB). |
114 |
94.2 |
|
General walk-in Clinic (GW). |
71 |
58.7 |
|
Chronic Disease Clinic (CDC). |
36 |
29.8 |
|
Antenatal Clinic (ANC). |
36 |
29.8 |
|
Well Women Clinic (WWC). |
11 |
9.1 |
|
Variable: |
Mean |
Standard deviation (SD) |
|
Age: |
33.60 |
9.08 |
|
Year of experience: |
7.19 |
7.64 |
(Table 2) Nearly all (97.5%) of the studied sample heard about EC. The EC method most heard about was the Levonorgestrel method (plan B method) and the IUCD copper method with 84.3% followed by the Levonorgestrel method (split method) with 72.7% while the method least heard about was Ulipristal method with 28.1% of the participants. Data is shown in table two.
Table 2. Hear about emergency contraception and its methods among the studied sample (n = 121).
|
Hear about: |
Yes. |
No. |
||
|
No. |
%. |
No. |
%. |
|
|
Emergency contraception. |
118 |
97.5 |
3 |
2.5 |
|
Yuzpe method. |
81 |
66.9 |
40 |
33.1 |
|
Levonorgestrel method (plan B method). |
102 |
84.3 |
19 |
15.7 |
|
Levonorgestrel method (split method). |
88 |
72.7 |
33 |
27.3 |
|
Ulipristal method. |
34 |
28.1 |
87 |
71.9 |
|
IUCD copper method. |
102 |
84.3 |
19 |
15.7 |
(Table 3) The most available EC method was the IUCD copper method with 60.3%, while the least available method was the Ulipristal method with only 5%. More than half of the sample was not sure about the availability of all methods. Data is shown in table three.
Table 3. Availability of emergency contraception methods.
|
Availability of emergency contraception methods: |
Yes |
No |
Not sure |
|||
|
No. |
% |
No. |
% |
No. |
% |
|
|
Yuzpe method. |
23 |
19.0 |
24 |
19.8 |
71 |
58.7 |
|
Levonorgestrel method. |
39 |
32.2 |
26 |
21.5 |
53 |
43.8 |
|
Ulipristal method. |
6 |
5.0 |
32 |
26.4 |
80 |
66.1 |
|
IUCD copper method. |
73 |
60.3 |
15 |
12.4 |
30 |
24.8 |
(Table 4) The highest scored reasons for EC indication were unprotected sexual intercourse by 90.9%, followed by Condom breakage by 83.5% of the participants. The Majority (77.7%) of the participated physicians know the correct time of initiating oral EC methods, and most of them have never been trained on the use and application of EC. Data is shown in table four.
Table 4. Knowledge about emergency contraception among the studied sample (n = 121).
|
Knowledge items: |
Correct answer |
Incorrect answer |
||
|
No. |
% |
No. |
% |
|
|
Pregnancy test necessary before prescribing EC. |
56 |
46.3 |
65 |
53.7 |
|
Per-vaginal (PV) examination necessary before prescribing EC. |
80 |
66.1 |
41 |
33.9 |
|
The (EC) acts as an abortifacient. |
96 |
79.3 |
25 |
20.7 |
|
Indications of EC: |
||||
|
Condom breakage. |
101 |
83.5 |
20 |
16.5 |
|
Rape. |
91 |
75.2 |
30 |
24.8 |
|
Missed contraceptive pills. |
82 |
67.8 |
39 |
32.2 |
|
Unprotected sexual intercourse. |
110 |
90.9 |
11 |
9.1 |
|
Unintended pregnancy. |
36 |
29.8 |
85 |
70.2 |
|
Failure of contraceptive use. |
43 |
35.5 |
78 |
64.5 |
|
The correct time for the initiation of oral EC methods. |
94 |
77.7 |
27 |
22.3 |
|
Oral EC that has proven effective for late intake. |
17 |
14.0 |
104 |
86.0 |
|
EC method that interferes with fertilization and prevents implantation. |
74 |
61.2 |
47 |
38.8 |
|
EC use discourages regular contraceptive-use. |
88 |
72.7 |
33 |
27.3 |
|
Have you been trained in the use of and application of EC? |
23 |
19.0 |
98 |
81.0 |
(Table 5) The results of the current study revealed that more than two thirds (67.8%) of the studied sample had unsatisfactory Knowledge about EC, while only 32.2% (less than the third) had satisfactory knowledge. Data is shown in table five.
Table 5. Levels of Knowledge about emergency contraception among the studied sample (n = 121).
|
Levels of knowledge: |
No. |
% |
|
Satisfactory. |
39 |
32.2 |
|
Unsatisfactory. |
82 |
67.8 |
(Table 6) As shown in table six, most (87.6%) of the studied sample had not prescribed EC before, while only 12.4% did so. All those who prescribed EC before have prescribed it rarely. More than half of the sample (53.7%) have never done so, while 28.1% were not sure, and only 18.2% prescribed EC.
Table 6. Practices regarding emergency contraception among the studied sample (n=121).
|
Practices regarding emergency contraception |
Answers |
No. |
% |
|
Have you ever prescribed an EC? |
Yes. |
15 |
12.4 |
|
No. |
106 |
87.6 |
|
|
If you have prescribed it before, how often typically prescribed the method? |
Rare. |
15 |
100.0 |
|
Would you refer a case to a gynecologist for the prescription of EC? |
Yes. |
22 |
18.2 |
|
No. |
65 |
53.7 |
|
|
Not sure. |
34 |
28.1 |
(Table 7) As shown in table seven, the item with the highest positive attitude was “Are you interested in learning more about EC with 57.9% strongly agree, and 33.9% agree, followed by benefits of EC outweigh the risks with 31.4% strongly agree, and 57% agree. On the other hand, the item with the highest negative attitude was “are you satisfied with your current knowledge of EC” with only 1.7% strongly agree and 13.2% agree. Most of the studied sample (38% strongly agree, and 43% agree) are in favor of the use of EC, and only 19% were either strongly agree or agree that they are uncomfortable with prescribing EC for religious/ethical reasons.
Table 7. Attitude towards emergency contraception among the studied sample (n = 121).
|
Attitude items: |
Strongly agree |
Agree |
Neutral |
Disagree |
Strongly disagree |
|||||
|
No. |
% |
No. |
% |
No. |
% |
No. |
% |
No. |
% |
|
|
1. The benefits of emergency contraception (EC) outweigh the risks. |
38 |
31.4 |
69 |
57.0 |
13 |
10.7 |
1 |
0.8 |
0 |
0.0 |
|
2. Emergency contraception (EC) appropriate for discussion at routine consultation. |
25 |
20.7 |
38 |
31.4 |
35 |
28.9 |
22 |
18.2 |
1 |
0.8 |
|
3. Are you satisfied with your current knowledge of emergency contraception? |
2 |
1.7 |
16 |
13.2 |
42 |
34.7 |
39 |
32.2 |
22 |
18.2 |
|
4. Are you interested in learning more about emergency contraception (EC)? |
70 |
57.9 |
41 |
33.9 |
8 |
6.6 |
2 |
1.7 |
0 |
0.0 |
|
5. Do you think emergency contraception (EC) should be more widely advertised? |
26 |
21.5 |
49 |
40.5 |
41 |
33.9 |
3 |
2.5 |
2 |
1.7 |
|
6. Do you feel uncomfortable prescribing emergency contraception (EC) for religious/ethical reasons? |
9 |
7.4 |
14 |
11.6 |
38 |
31.4 |
35 |
28.9 |
25 |
20.7 |
|
7. Are you concerned about legal liability when you prescribe emergency contraception (EC)? |
14 |
11.6 |
35 |
28.9 |
37 |
30.6 |
28 |
23.1 |
7 |
5.8 |
|
8. Are you with the use of emergency contraception (EC)? |
46 |
38.0 |
52 |
43.0 |
20 |
16.5 |
3 |
2.5 |
0 |
0.0 |
(Table 8) Overall, most (67.8%) of the studied sample had a positive attitude towards EC, while only 32.2% (less than the third) showed a negative attitude, as shown in table eight.
Table 8. Levels of attitude among the studied sample (n = 121).
|
Levels of attitude: |
No. |
% |
|
Positive |
82 |
67.8 |
|
Negative |
39 |
32.2 |
(Table 9) There was a statistically significant difference between health care providers’ knowledge and attitude towards EC with a p-value of 0.002. Among those with unsatisfactory knowledge level, 41.5% have a negative attitude towards EC, while 58.5% showed a positive attitude. For those with a satisfactory level of knowledge, the percent of negative attitude was only 12.8%, while the majority (87.2%) have a positive attitude. Data is shown in table nine.
Table 9. Relation between knowledge and attitude towards emergency contraception among the studied sample (n=121).
|
Levels of knowledge: |
Levels of attitude: |
Chi-square |
p-value |
|||
|
Positive. |
Negative. |
|||||
|
No. |
% |
No. |
% |
|||
|
Satisfactory. |
34 |
87.2 |
5 |
12.8 |
9.92 |
0.002* |
|
Unsatisfactory. |
48 |
58.5 |
34 |
41.5 |
||
|
*significant at p-value <0.05 |
||||||
(Table 10) As shown in table ten, there was no statistically significant difference between health care providers’ knowledge and practice of EC with the p-value was 0.2. Among those with satisfactory knowledge level, the percent of prescribed EC was only 17.9%, while the majority (82.1%) have not prescribed EC. For those with unsatisfactory knowledge level, 9.8% prescribed EC while 90.2% have not prescribed EC.
Table 10. The relation between knowledge and practice of emergency contraception among the studied sample (n = 121).
|
Levels of knowledge: |
The Practice of EC: |
Chi-square: |
p-value: |
|||
|
YES |
NO |
|||||
|
No. |
% |
No. |
% |
|||
|
Satisfactory. |
7 |
17.9 |
32 |
82.1 |
1.63 |
0.2 |
|
Unsatisfactory. |
8 |
9.8 |
74 |
90.2 |
||
(Table 11) There was no statistically significant difference between health care providers’ practice of and attitude towards EC since the p-value was 0.09. Among those with a Positive attitude, the percent of prescribed EC was only 15.9%, while the majority (84.1%) have not prescribed EC. For those with a negative attitude, 5.1% prescribed EC while 94.9% have not prescribed EC. Data is shown in table eleven.
Table 11. The relation between practice of and attitude towards emergency contraception among the studied sample (n=121).
|
Attitude |
The Practice of EC: |
Chi-square: |
p-value: |
|||
|
Yes |
No |
|||||
|
No. |
% |
No. |
% |
|||
|
Positive. |
13 |
15.9 |
69 |
84.1 |
2.8 |
0.09 |
|
Negative. |
2 |
5.1 |
37 |
94.9 |
||
(Table 12) As shown in table twelve, there was no statistically significant difference in levels of EC Knowledge by gender, nationality, marital status, position in the medical profession, place of highest qualification achieved and area covered by physicians since the p-value was more than 0.05.
Table 12. Demographic characteristics and occupational history According to Knowledge of emergency contraception among the studied sample (n = 121).
|
Items: |
Level of knowledge |
P-value: |
|||
|
Satisfactory |
Unsatisfactory |
||||
|
No. |
% |
No. |
% |
||
|
Gender: |
|||||
|
Male. |
20 |
32.3 |
42 |
67.7 |
0.99 |
|
Female. |
19 |
32.2 |
40 |
67.8 |
|
|
Nationality: |
|||||
|
Saudi. |
27 |
29.3 |
65 |
70.7 |
0.227 |
|
Non-Saudi. |
12 |
41.4 |
17 |
58.6 |
|
|
Marital status: |
|||||
|
Single. |
8 |
20.5 |
31 |
79.5 |
0.084 |
|
Married. |
31 |
38.8 |
49 |
61.3 |
|
|
Widow. |
0 |
0 |
2 |
100 |
|
|
Position in medical profession: |
|||||
|
Consultant. |
1 |
9.1 |
10 |
90.9 |
0.066 |
|
Senior registrar. |
13 |
50.0 |
13 |
50.0 |
|
|
Registrar. |
10 |
45.5 |
12 |
54.5 |
|
|
Senior house officer. |
2 |
33.3 |
4 |
66.7 |
|
|
Senior resident. |
6 |
25.0 |
18 |
75.0 |
|
|
Junior resident. |
7 |
21.9 |
25 |
78.1 |
|
|
Highest qualification achieved in: |
|||||
|
National. |
28 |
29.8 |
66 |
70.2 |
0.518 |
|
International, but not Western. |
7 |
43.8 |
9 |
56.3 |
|
|
Western. |
4 |
36.4 |
7 |
63.6 |
|
|
The area covers most of the times: |
|||||
|
General booked Clinic GB. |
36 |
31.6 |
78 |
68.4 |
0.403 |
|
General walk-in Clinic GW. |
23 |
32.4 |
48 |
67.6 |
0.562 |
|
Chronic Disease Clinic CDC. |
21 |
33.3 |
24 |
66.7 |
0.513 |
|
Antenatal Clinic ANC. |
6 |
31.6 |
13 |
68.4 |
0.588 |
|
Well Women Clinic WWC. |
4 |
36.4 |
7 |
63.6 |
0.498 |
|
Age (years) |
34.36+8.264 |
33.24+9.475 |
0.530 |
||
| leftYears of experience Mean+ stander deviation. |
7.179+6.613 |
7.195+8.125 |
0.992 |
||
| leftNumber of sessions per week Mean+ stander deviation. |
6.821+2.846 |
6.988+2.401 |
0.737 |
||
(Table 13) As shown in table thirteen, Statistically significant results were obtained between the practice of EC with nationality (chi-square=17.13), position in the medical profession (chi-square=14.34), highest qualification achieved (chi-square=7.72), and area of specialization; being the highest among Non-Saudis, registrars, those with Western high qualifications, covering general walk-in clinic GW (chi-square=8.48), Antenatal clinic ANC (chi-square=7.63), and Well Women Clinic WWC (chi-square=6.40) with p-values of <0.05. The percentage of primary health care physicians who prescribed emergency contraception was 15/121 (12.4%). The percentages of Non-Saudi physicians and Saudi physicians who prescribed EC were 34.5% and 5.4%; respectively.
Table 13. Demographic characteristics and occupational history According to the practice of emergency contraception among the studied sample (n = 121).
|
Items: |
The Practice of EC: |
P-value: |
|||
|
Yes |
No |
||||
|
No. |
% |
No. |
% |
||
|
Gender: |
|||||
|
Male. |
4 |
6.5 |
58 |
93.5 |
0.990 |
|
Female. |
11 |
18.6 |
48 |
81.4 |
|
|
Nationality: |
|||||
|
Saudi. |
5 |
5.4 |
87 |
94.6 |
0.000* |
|
Non-Saudi. |
10 |
34.5 |
19 |
65.5 |
|
|
Marital status: |
|||||
|
Single. |
1 |
2.6 |
38 |
97.4 |
0.059 |
|
Married. |
14 |
17.5 |
66 |
82.5 |
|
|
Widow. |
0 |
0 |
2 |
100 |
|
|
Position in medical profession: |
|||||
|
Consultant. |
3 |
27.3 |
8 |
72.7 |
0.014* |
|
Senior registrar. |
1 |
3.8 |
25 |
96.2 |
|
|
Registrar. |
7 |
31.8 |
15 |
68.2 |
|
|
Senior house officer. |
1 |
16.7 |
5 |
83.3 |
|
|
Senior resident. |
1 |
4.2 |
23 |
95.8 |
|
|
Junior resident. |
2 |
6.3 |
30 |
93.8 |
|
|
Highest qualification achieved in: |
|||||
|
National. |
8 |
8.5 |
86 |
91.5 |
0.021* |
|
International, but not Western. |
3 |
18.8 |
13 |
81.3 |
|
|
Western. |
4 |
36.4 |
7 |
63.6 |
|
|
The area covers most of the times: |
|||||
|
General booked Clinic GB. |
15 |
13.2 |
99 |
86.8 |
0.305 |
|
General walk-in Clinic GW. |
14 |
19.7 |
57 |
80.3 |
0.004* |
|
Chronic Disease Clinic CDC. |
7 |
19.4 |
29 |
80.6 |
0.140 |
|
Antenatal Clinic ANC. |
6 |
31.6 |
13 |
68.4 |
0.014* |
|
Well Women Clinic WWC. |
4 |
36.4 |
7 |
63.6 |
0.030* |
|
Age (years) |
43.666+10.540 |
32.179+7.934 |
0.530 |
||
|
Years of experience |
15.400+10.048 |
6.028+6.503 |
0.992 |
||
|
Number of sessions per week |
8.200+2.144 |
6.754+2.551 |
0.737 |
||
|
*significant at p-value <0.05 |
|||||
(Table 14) There was no statistically significant difference between attitude towards EC by gender, nationality, marital status, position in the medical profession, highest qualification, area covered (general booked clinic GB and Chronic Disease Clinic CDC) age, years and number of sessions per week since all p-values were >0.05. In contrast, a statistically significant difference (p-value <0.05) has been found between attitude towards EC and General Clinic walk-in GW (chi-square=5.40), Antenatal Clinic ANC (chi-square=4.86), Well Women Clinic WWC (chi-square=5.75). The percentages of primary health care physicians with a positive attitude who were covering General walk-in Clinic GW, Antenatal Clinic ANC, Well Women Clinic WWC were 76.1%, 89.5 %, and 100% respectively. Physicians with a positive attitude had a borderline (t-test=1.91, P 0.052) statistically significant higher mean (±SD) of years of experience compared to those with a negative attitude at 8.09+8.279 vs. 5.28+5.730; respectively. Data is shown in table fourteen.
Table 14. Demographic characteristics and occupational history according to attitude towards emergency contraception among the studied sample (n = 121).
|
Items: |
Level of attitude: |
P value: |
|||
|
Positive. |
Negative. |
||||
|
No. |
% |
No. |
% |
||
|
Gender: |
|||||
|
Male. |
37 |
59.7 |
25 |
40.3 |
0.065 |
|
Female. |
45 |
76.3 |
14 |
23.7 |
|
|
Nationality: |
|||||
|
Saudi. |
60 |
65.2 |
32 |
34.8 |
0.367 |
|
Non-Saudi. |
22 |
75.9 |
7 |
24.1 |
|
|
Marital status: |
|||||
|
Single. |
22 |
56.4 |
17 |
43.6 |
0.130 |
|
Married. |
58 |
72.5 |
22 |
27.5 |
|
|
Widow. |
2 |
100 |
0 |
0 |
|
|
Position in medical profession: |
|||||
|
Consultant. |
7 |
63.6 |
4 |
36.4 |
0.060 |
|
Senior registrar. |
23 |
88.5 |
3 |
11.5 |
|
|
Registrar. |
17 |
77.3 |
5 |
22.7 |
|
|
Senior house officer. |
4 |
66.7 |
2 |
33.3 |
|
|
Senior resident. |
12 |
50.0 |
12 |
50.0 |
|
|
Junior resident. |
19 |
59.4 |
13 |
40.6 |
|
|
Highest qualification achieved in: |
|||||
|
National. |
63 |
67.0 |
31 |
33.0 |
0.782 |
|
International, but not Western. |
12 |
75.0 |
4 |
25.0 |
|
|
Western. |
7 |
63.6 |
4 |
36.4 |
|
|
The area covers most of the times: |
|||||
|
General booked Clinic GB. |
78 |
68.4 |
36 |
31.6 |
0.403 |
|
General walk-in Clinic GW. |
54 |
76.1 |
17 |
23.9 |
0.017* |
|
Chronic Disease Clinic CDC. |
21 |
58.3 |
15 |
41.7 |
0.110 |
|
Antenatal Clinic ANC. |
17 |
89.5 |
2 |
10.5 |
0.021* |
|
Well Women Clinic WWC. |
11 |
100 |
0 |
0 |
0.016* |
|
Age (years) |
34.52+9.399 |
31.67+8.154 |
0.106 |
||
|
Years of experience |
8.09+8.279 |
5.28+5.730 |
0.052 |
||
|
Number of sessions per week |
7.036+2.550 |
6.72+2.543 |
0.522 |
||
|
*significant at p-value <0.05 |
|||||
(Table 15) The results of the current study highlighted that 82.6% of physicians participated in the current study perceived lack of knowledge as the most important barrier of EC. Cultural issues came in second place with 64.5% while patients’ acceptance was next with 35.5% and side effects of methods with 22.3%. Only 1.7% perceived unavailability in pharmacies as a barrier. Data is shown in table fifteen. Although nearly all the studied sample (97.5%) heard about EC, the knowledge about EC was moderate, with total knowledge of 58.5% and less than one-third of the sample had a satisfactory knowledge level. Participated physicians mostly did not hear about some EC methods such as the Ulipristal method.
Table 15. Perceived barriers of emergency contraception among the studied sample (n = 121).
|
Perceived barriers of EC: |
No. |
% |
|
Lack of knowledge |
100 |
82.6 |
|
Patients acceptance |
43 |
35.5 |
|
Cultural issues |
78 |
64.5 |
|
Side effects of methods |
27 |
22.3 |
Discussion
The results of the current study are in accordance with previous similar studies [25–28], which have shown clear gaps in knowledge regarding emergency contraception among healthcare providers, including physicians. This might have an effect on the provision of emergency contraception as they are involved in management, and incomplete knowledge could delay timely scheduling or administration. On the other hand, such findings were in contrast with what has been reported from Lagos [29], where a high degree of awareness of and a largely favorable disposition toward emergency contraceptives among health care providers was shown. The copper IUD, being the most available EC method according to physicians participated in the current study, is by far the most effective option for EC; since a review of 42 studies showed that the pregnancy rate after insertion of the copper IUD for EC is less than 0.1% [30].
Lack of training on the use and application of EC was reported by most of the physicians, which reflects the shortage of dependable information on EC in Saudi Arabia. This was also previously reported from a similar study from Vietnam [31]. It seems that the gaining of EC knowledge during pre- and in-service education of healthcare providers in Saudi Arabia is not served. Additionally, most of the participants reported that they were unsatisfied with their current knowledge of emergency contraception. Proper training is urgently needed to ensure that physicians are knowledgeable enough with different methods of EC to prescribe it when the situation warrants.
A higher knowledge about EC will build up health care professionals’ capacity to provide accurate and effective information on EC to prevent unplanned and unwanted pregnancies. Similar studies in Korea and America found a significantly higher knowledge of EC among participants who had received education and formal content on EC [32,33]. As per the results of the current study, EC still remains a mostly underutilized option in unplanned pregnancy prevention. The knowledge gap is almost the main reason for both the health care providers, which can negatively impact the prescribing habits and future promotion of EC, and this is in agreement with the Sharma C study [34]. In disagreement with the Gupta R et al. study from India [35], the highest proportion of primary care physicians in our study “disagree” on the point “didn’t feel uncomfortable prescribing EC on religious or ethical grounds”.
According to the United Nations Fund for Population Activities (UNFPA 2013), emergency contraception acts on disrupting ovulation and reduces pregnancy likelihood. It cannot prevent fertilized egg implantation, harm a developing embryo, or end a pregnancy. Additionally, according to the WHO, there is no risk on the fetus if a pregnant woman uses the EC. Based on this, performing a pregnancy test before prescribing these methods is not necessary [36]. However, only less than half (46.3%) of participants in the current study had correct knowledge in this regard, a percentage which is considered lower compared to a rate of 67% that was reported by the study of Abdulghani and colleagues in Pakistan [25], and a rate of 94% in an Iranian study [37].
Nonetheless, the majority (79.3%) of the physicians in this study wrongly agreed that EC is an abortifacient which is far higher than the findings of Lee et al. in America [38], and Delaram and Rafie in Iran [39]. These are alarming findings, given that women seeking to use EC depend on healthcare providers for information. This emphasizes the need to broaden and provide detailed education on EC in medical training schools. Moreover, it was worrying about finding that the physicians participated in the current study believed EC use discourage usual contraceptives use, which is against the literature that does not support the argument that EC use discourages the use of other methods of contraception [40].
Compared to a previous similar study from Iran which reported that 95.7% of the health care providers had a positive attitude toward EC, the current study showed that 67.8% of the respondents have a positive attitude towards EC [37]. More than half of the participants felt that emergency contraception was an appropriate topic to discuss at routine consultation, a finding which is in contrast to the Pakistani study, where more than half of the participants felt that EC was not an appropriate topic to discuss at routine consultation. The largest percentage of the participants in our study were not uncomfortable because of religious reasons, which is different from the findings of previous research [25,41,42].
Lower levels of EC prescription have been reported from studies from developing countries. In Nairobi, Kenya, 15% of family-planning service providers reported having prescribed EC [43], and 20% of primary healthcare workers EC in Turkey [44,45]. These rates are even considered high compared to what we found in our study, where the prescription rate was 12.4%.
To the best of our knowledge, this is the first study conducted among primary health care physicians in this regard. Previous studies conducted among Saudi women and came up with the findings that the knowledge, awareness, and use of EC among Saudi women was low; however, a positive attitude for future EC use exists [46,47]. Though it is a small study with small sample size, further larger studies, at regional levels, can identify geographic and demographic gaps in EC practices. It would also be recommended to examine the knowledge and practices of other healthcare providers, including nurses and midwives, who may offer education to patients and communities about emergency contraception.
Conclusion
This study showed clear gaps in emergency contraception (EC) knowledge among primary healthcare physicians. Although the vast majority of the participants heard about EC, their knowledge was moderate, and less than one third had a satisfactory knowledge level. Most of the participants showed a positive attitude towards learning more about EC and also showed that they are with the use of EC. Educational programs that enhance and promote physicians’ awareness of and attitude toward emergency contraception is highly recommended.
Recommendations
Educational efforts should be focused on training of healthcare providers to improve correct access of women and effective use of different emergency contraception methods. Such educational efforts should focus on providing specific knowledge, with particular attention to correct common misconceptions about the EC methods. Providers should be encouraged to inform all potential users about the methods and to prescribe it to clients who require it. Communication about emergency contraception would also provide opportunities for counseling on long-term contraceptive needs. Discussion about emergency contraception should be raised during routine health check-up visits of women. Besides the use of different educational methods to enhance awareness and attitudes of providers, barriers for using EC should be identified, and trials to eliminate them should be done. Future research should be directed at implementing interventions to enhance these types of discussions.
Ethical Considerations
Ethical approval of research conduction from the Research Ethics Committee, Medical Services Department for Armed Forces was approved on 7 MARCH 2018 project no: 1043. It was an amendment and has been approved by the Research Ethics Committee on 09 April 2019. The verbal consent was taken from each physician after explained to them the aim and objectives of the study. The study did not include treatment or intervention for participants. Confidentiality was maintained during data collection and usage.
References
- Yazdkhasti M, Pourreza A, Pirak A, Abdi F (2015) Unintended Pregnancy and Its Adverse Social and Economic Consequences on Health System: A Narrative Review Article. Iranian Journal of Public Health 44: 12–21.
- JUVENILES AT RISK (2016) International Journal of Social Impact 1: 17.
- Roudi-Fahimi F, Monem AA (2010) Unintended pregnancies in the Middle East and North Africa (Washington, DC: PRB, 2010). Available from: http://www.Igwg.Org/pdf10/unintended pregnancies.Pdf. Accessed on 14.01.2013.
- Dabash R, Roudi-Fahimi F (2014) Abortion in the Middle East and North Africa population reference bureau. Available from: http://www.Prb.Org/pdf08/menaabortion.Pdf. Accessed on 27 Nov. 2014.
- World health organization. Unsafe abortion (2003) Global and regional estimates of the incidence of unsafe abortion and associated mortality in 2003. 5th edn. Geneva: World Health Organization; 2007. http://whqlibdoc.Who.Int/publications/2007/9789241596121_eng.Pdf.
- World Health Organization: Contraception: Issues in adolescent health and development. Geneva: World Health Organization; 2004. http://whqlibdoc.who.int/publications/2004/9241591447.
- Neinstein LS, Gordon MC, Katzman KD, Rosen SD, Woods RE (2008) Adolescent health care: a practical guide. Philadelphia: Lippincott Williams and Wilkins; Pg No: 533–649.
- Aksu H, Kucuk M, Karaoz B, Ogurlu N (2010) Knowledge and attitude of health care providers working in primary health care units concerning emergency contraception. Gynecol Obstet Invest 70: 179–185.
- Szarewski A, Guillebaud J (2002) Contraception: a user’s guide. 3rd Edn. New York: Oxford University Press.
- Mohammed S, Hossain I, Khan ME, Rahman M, Sabastian MP (2005) Emergency contraceptive pills. South East Asia Regional training manual USAID, Population Council Frontiers; Pg No: 19–30.
- Gemzell-Danielsson K (2010) Mechanism of action of emergency contraception. Contraception 82: 404–409.
- Mangiaterra V, Pendse R, Mclure K, Rosen J (2008) Adolescent pregnancy. Department of making pregnancy safer (MPS). WHO MPS note 2008: 1.
- Gemzell-Danielsson Kristina, Berger Cecia. PGL, Lalit Kumar (2013) Emergency contraception- Mechanism of action. Contraception 87: 300–308.
- Shaaban OM, Fathalla MM, Shahin AY, Nasr A (2011) Emergency contraception in the context of marriage in Upper Egypt. Int J Gynecology Obstet 112: 195–199.
- Shoveller J, Chabot C, Soon JA, Levine M (2007) Identifying barriers to emergency contraception use among young women from various socio-cultural groups in British Columbia, Canada. Perspect Sex Reprod Health 39: 13–20.
- Abbott J, Feldhaus KM, Houry D, Lowenstein SR (2004) Emergency contraception: what do our patients know? Ann Emerg Med 43: 376–381. [crossref]
- Marafie N, Ball D, Abahussain E (2007) Awareness of hormonal emergency contraception among married women in a Kuwaiti family social network. EJOG Reprod Biol 130: 216–222.
- El-Sabaa HA, Ibrahim AF, Hasan WA (2013) Awareness and use of emergency contraception among women of childbearing age at the family care centers in Alexandria, Egypt. J Taibah Univ Med Sci 8: 167- 172.
- Abdulghani H, Karim S, Irfan F (2009) Emergency Contraception: Knowledge and Attitudes of Family Physicians of a Teaching Hospital, Karachi, Pakistan. Journal of health, population and nutrition 27: 339–344.
- Ibrahim Z, Ahmed M, Shaaban M (2013) Knowledge, attitude and practice of emergency contraception among health care providers in Ismailia, Egypt. Middle East Fertility Society Journal 18: 246–252.
- Bildircin M, Sahin N (2005) Knowledge, attitudes and practices regarding emergency contraception among family-planning providers in Turkey. he European Journal of Contraception and Reproductive Health Care 10: 151–156.
- Karim SI, Irfan F, Al-Rowais N, Al-Zahrani B, Qureshi R, et al. (2015) Emergency contraception: Awareness, attitudes and barriers of Saudi Arabian Women. Pak J Med Sci 31: 1500–1505.
- Knowledge and attitude about emergency contraception among Saudi women of childbearing age. – PubMed – NCBI [Internet]. [cited 2019 Aug 5].Available from: https://www.ncbi.nlm.nih.gov/pubmed/30911479
- Mohammad-Alizadeh-Charandabi S, Farshbaf-Khalili A, Moeinpoor R (2012) Emergency Contraception: Providers’ Knowledge and Attitudes and Their Relationship with Users’ Knowledge and Attitudes at Public Health Centers/Posts of Tabriz. J Caring Sci 1: 53–59.
- Abdulghani HM, Karim SI, Irfan F (2009) Emergency Contraception: Knowledge and Attitudes of Family Physicians of a Teaching Hospital, Karachi, Pakistan. J Health Popul Nutr 27: 339–344.
- Adekunle AO, Arowojolu AO, Adedimeji AA, Okunlola MA (2000) Emergency contraception: survey of knowledge, attitudes and practice of health care professionals in Ibadan, Nigeria. J ObstetrGynaecol 20: 284–289.
- Sable MR, Schwartz LR, Kelly PJ, Lisbon E, Hall MA (2006) Using the theory of reasoned action to explain physician intention to prescribe emergency contraception. Prespect Sex Reprod Health 38: 20–27.
- Ebuehi OM, Ebuehi OA, Inem V (2006) Health care providers’ knowledge of, attitudes toward and provision of emergency contraceptives in Lagos, Nigeria. IntFami-lyPlannPerspect 32: 89–93.
- Ebuehi OM, Ebuehi OAT, Inem V (2006) Health care providers’ knowledge of, attitudes toward and provision of emergency contraceptives in Lagos, Nigeria. IntFam Plan Perspect 32: 89–93.
- Cleland K, Zhu H, Goldstuck N, et al. (2012) The efficacy of intrauterine devices for emergency contraception: A systematic review of 35 years of experience. Human Reproduction 27: 1994–2000.
- Ngoc N, Ellertson C, Surasrang Y, Thai Loc L (1997) Knowledge and Attitudes about Emergency Contraception among Health Workers in Ho Chi Minh City, Vietnam. International Family Planning Perspectives 23: 68.
- Kang HS1, Moneyham L (2008) Use of emergency contraceptive pills and condoms by college students: a survey. Int J Nurs Stud 45: 775–783. [crossref]
- Lee CJ, Ahonen K, Apling M, Bork C (2012) Emergency contraception knowledge among nurse practitioner students. J Am Acad Nurse Pract 24: 604–611.
- Sharma C (2017). Understanding of emergency contraception among nursing staff in a tertiary care hospital of Andaman and Nicobar Islands, India. J Basic ClinReprod Sci 6: 133–136.
- Gupta R, Langer B, Singh P, Kumari R, Akhtar N, et al. (2018) Health care providers knowledge, attitudes and perceived barriers towards emergency contraception in a sub-Himalayan state of India. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 7: 3244.
- World Health Organization Department of Repro-ductive Health and Research (WHO/RHR) (2008) Johns Hopkins Bloomberg School of Public Health /Center for Communication Program (CCP), Info Project.Family planning: a global handbook for providers. Baltimore and Geneva: CCP and WHO; PG No: 53.
- Mohammad-Alizadeh-Charandabi S, Farshbaf-Khalili A, Moeinpoor R (2012) Emergency Contraception: Providers’ Knowledge and Attitudes and Their Relationship with Users’ Knowledge and Attitudes at Public Health Centers/Posts of Tabriz. Journal of Caring Sciences 1: 53.
- Lee CJ, Ahonen K, Apling M, Bork C (2012) Emergency contraception knowledge among nurse practitioner students. Journal of the American Academy of Nurse Practitioners 24: 604–611.
- Delaram M, Rafie H (2012) Knowledge and attitudes of emergency contraception among medical sciences students. Futur Med Educ J 2: 9–13.
- Mohammed S, Abdulai A-M, Iddrisu OA (2019) Pre-service knowledge, perception, and use of emergency contraception among future healthcare providers in northern Ghana. ContraceptReprod Med [Internet] Jan 24 [cited 2019 Aug 4]: 4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6345032/
- Corbett PO, Mitchell CP, Taylor JS, Kemppainen J (2006) Emergency contraception: knowledge and perceptions in a university population. J Am Acad Nurse Pract 18: 161–168.
- Xu X, Vahratian A, Patel DA, McRee AL, Ransom SB (2007) Emergency contraception provision: a survey of Michigan physicians from five medical specialties. J Women Health (Larchmt) 16: 489–498.
- Muia E1, Ellertson C, Lukhando M, Flul B, Clark S, et al. (1999) Emergency contraception in Nairobi, Kenya: knowledge, attitudes and practices among policymakers, family planning providers and clients, and university students. Contraception 60: 223–232. [crossref]
- Mandiracioglu A, Mevsim V, Turgul O (2003). Health personnel perceptions about emergency contraception in primary health-care centers. Eur J ContraceptReprod Health Care 8: 145–149.
- Bildircin M, Sahin NH (2005) Knowledge, attitudes and practices regarding emergency contraception among family-planning providers in Turkey. Eurp J ContraceptReprod Health Care 10:151–156.
- Journal of Family Medicine and Primary Care – Knowledge and attitude about emergency contraception among Saudi women of childbearing age?: Download PDF [Internet]. [cited 2019 Aug 4]. Available from: http://www.jfmpc.com/downloadpdf.asp?issn=22494863; year=2019;volume=8;issue=1;spage=44;epage=48;aulast=Alharbi;type=2
- Karim SI, Irfan F, Rowais NA, Zahrani BA, Qureshi R, et al. (2015) Emergency contraception: Awareness, attitudes and barriers of Saudi Arabian Women. Pak J Med Sci 31: 1500–1505.